Retinal vein thrombosis خثار الوريد الشبكي في العين
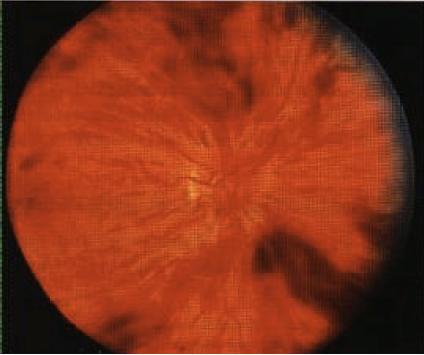
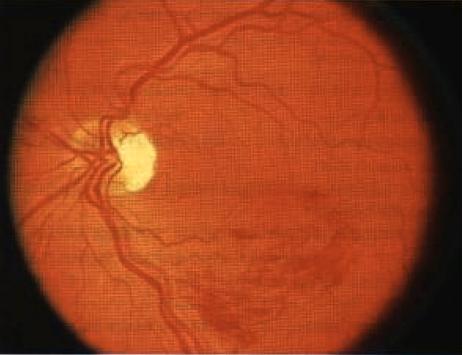
INSTRUCTION Examine this patient's eyes. Examine this patient's fundus. SALIENT FEATURES History · Branched retinal vein occlusion: decreased vision, floaters suggest vitreal haemorrhage. · Central retinal vein occlusion: loss of or decreased vision, headache (associated increase in intraocular pressure), floaters. · History of hypertension, diabetes, glaucoma, multiple myeloma or macro-globulinaemia. Examination Patient I has central retinal vein occlusion (Fig. 80), i.e. occlusion is behind the cribriform plate: · Multiple retinal and preretinal haemorrhages surround the optic nerve head. There is marked dilatation and tortuosity of the veins, hyperaemia or oedema of the nerve head and soft exudates - 'blood and thunder' appearance. · Visual acuity is only slightly reduced. Patient 2 has branch vein occlusion (Fig. 81); the occlusion is in front of the cribriform plate Occlusion occurs just distal to the arteriovenous crossing. The superior temporal vein is most commonly involved. Haemorrhages are seen surrounding the occluded vein. · May cause a quadrantic field defect. · Visual prognosis is good if the haemorrhages do not extend to the macula with accompanying macular oedema. Proceed as follows: Tell the examiner that you would like to check for the following conditions: · Hypertension. · Chronic simple glaucoma. · Hyperviscosity syndromes (Waldenstrom's macroglobulinaemia, multiple myeloma). DIAGNOSIS This patient has multiple retinal haemorrhages (lesions) due to central retinal vein occlusion with underlying diabetes mellitus (aetiology). ADVANCED-LEVEL QUESTIONS What are the usual sites of occlusion in branch retinal vein occlusion? · At arteriovenous crossings, causing classical quadrantic or small macular occlusions. · Along the main veins, as in diabetes mellitus. · At the edges of the optic disc, resulting in occlusion of the hemisphere. · Peripherally, as in sickle cell disease. What are the vascular responses to retinal vein occlusion? These include dilatation of retinal capillaries, abnormal vascular permeability and retinal capillary closure. What is the prognosis in branch retinal vein occlusion? It varies from complete resolution with no residual visual deficits to a progressive deterioration resulting in permanent loss of vision. What is the clinical course in central retinal vein occlusion? · In mild cases, there is minimal dilatation of veins and haemorrhages with little no oedema of the macula and no visual deficit. · In severe instances, the vision may deteriorate to hand motions, with extensive deep and superficial haemorrhages with stagnation of blood in the markedly dilated veins and several cottonwool spots. What are the complications of central retinal vein occlusion? These include neovascularization of the retina, rubeosis iridis (usually visible by 1 month) and rubeotic glaucoma (usually by 3 months). How would you manage such eyes? · Treat the underlying condition. · Fluorescein angiography to determine areas of retinal ischaemia. · Regular follow-up by the ophthalmologist as secondary neovascularization is a common sequela and may need laser therapy. Panretinal photocoagulation prevents dreaded complication of neovascular glaucoma. I (b. 1906), Medicine, Oppsala University, J.G. Waldenstrbm Professor of Sweden.